Better Your Sleep Hygiene For Fast Weightloss Today!

Having Trouble Falling To Sleep? Is Weight Loss Tied to Your Sleep Habits?
Ever wondered if your sleep patterns influence your weight? Statistics show that in 2021, 45% of U.S. adults slept less than 7 hours per night, a trend linked to increased body mass index and obesity rates.
Here I have also discussed about impact of physical activity on sleep quality. Learn how sleep shares an intricate relationship with your body weight, and explore how insufficient sleep disrupts appetite regulation and contributes to weight gain. Additionally, you get to gain insights into the bidirectional relationship between sleep and obesity.
To top it off I have provided you with a list of tested and proven practical tips for quality sleep to aid your fast weightloss journey.
Ready to transform your sleep and health? Explore the full article for in-depth insights and expert advice. Prioritize your sleep for a healthier version of you.
Is Weight Loss Connected To Sleep Health?
In 2021, 45% of U.S. adults aged 18 to 60 slept less than seven hours per day on weekdays, falling below the recommended duration for optimal health.
In recent decades, as the average duration and quality of sleep among Americans have declined, a parallel trend has emerged – an increase in average Body Mass Index (BMI) and elevated rates of obesity. Researchers have delved into the potential connections between sleep and weight, leading to a growing body of evidence suggesting that the quality and quantity of sleep play a significant role in metabolic health, weight gain, and the risk of obesity.
Several studies have illuminated the intricate relationship between sleep and weight. One key finding is the positive correlation between good sleep and a fast weightloss. The dynamics of this connection, however, are complex and multifaceted. Furthermore, disrupted sleep and weight gain is linked to metabolic disorders.
Research by National Library of Medicine (NLM) highlights a correlation between quality sleep and a healthy BMI. Further studies aim to unravel the complex details of this connection, with the goal of improving weight loss strategies and reducing obesity rates. Prioritizing on sleep is mandatory to manage weight and to gain up on your overall well-being.
Beyond the quantity of sleep, sleep quality is equally important and has a role in successful weight management. Disrupted sleep patterns, frequent awakenings, and conditions like sleep apnea or weight loss can negatively impact metabolic health. Poor sleep and weight gain is interrelated. Poor sleep quality increases insulin resistance. In this condition your body’s cells become less responsive to the hormone insulin. Further this elevates your blood glucose levels and this increases your chances to gain weight.
How Is Sleeplessness Related To Increase In Appetite?
Insufficient sleep may disrupt the delicate balance of neurotransmitters and hormones, such as ghrelin and leptin, central to appetite regulation. Studies show that sleep-deprived individuals have trouble falling to sleep and experience an increase in ghrelin, promoting hunger, and a decrease in leptin, which signals fullness. This imbalance leads to heightened appetite and reduced feelings of satiety, potentially contributing to weight gain.
Moreover, sleep deprivation influences food preferences, with individuals tending to choose calorie-rich and carbohydrate-laden options. The intricate connection between sleep and appetite regulation involves the body’s endo-cannabinoid system and orexin, suggesting a complex neurobiological relationship.
Researchers emphasize the need for further studies to unravel the nuances of this relationship between fast weightloss and sleep. Understanding how sleeplessness impacts neurotransmitter regulation is crucial in addressing the mechanisms behind increased appetite and its potential contribution to sustained weight gain.
What Is The Adequate Daily Dosage of Sleep?
Sleep deprivation, a common issue, can stem from various reasons, including health conditions. Recognizing changes in sleep patterns is crucial. The average daily sleep requirement varies with age:
- Adults and Elderly (18 years and up): 7 hrs to 9 hrs
- Teenagers (13 to 18 years): 8 hrs of sleep to 10 hrs
- Children (6 to 12 years): 9 hrs to 12 hrs
- Toddlers and Young children (1 to 5 years): 10 hrs of sleep to 14 hrs
- Newborns (3 months): 14 hrs to 17 hrs
- Infants (4 to 12 months): 12 hrs to 16 hrs
Individual needs may vary, but sudden or gradual changes in sleep patterns warrant attention. Sleep deprivation manifests differently—some struggle falling to sleep or to stay asleep, while others experience poor sleep quality, both impacting overall well-being. Note that you should seek guidance from your trusted healthcare practitioner if your sleep disturbances persist for a recurrent period of time.
Symptoms of Sleep Deprivation
Sleep deprivation leads to various symptoms, including:
- Slowed reaction times
- Irritability
- Fatigue
- Daytime sleepiness
- Headaches
- Difficulty thinking, focusing, and remembering
These sleep deprived symptoms can worsen and lead to severity in symptoms like – ptosis or drooping eyelid, hallucinations, tremors (hand) or impulsiveness in behavior.
4 Stages of Sleep Deprivation: How Does It Progress?
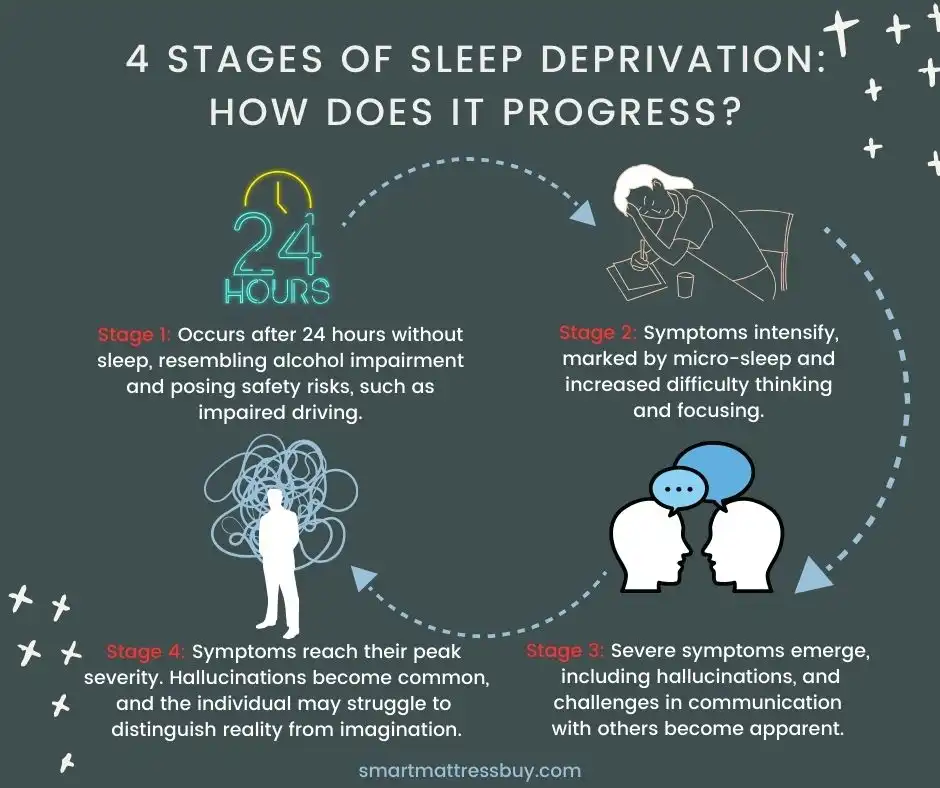
Now that I have covered information about the symptoms of a sleep deprived body, let’s learn how sleep deprivation progresses.
- Stage 1: Occurs after 24 hours without sleep, and posing safety risks, such as impairment in senses.
- Stage 2: Symptoms intensify, marked by micro-sleeps and increased difficulty thinking and focusing.
- Stage 3: Severe symptoms emerge, including hallucinations, and challenges in communication with others become apparent.
- Stage 4: Symptoms reach their peak severity. Hallucinations become common, and the individual may struggle to distinguish reality from imagination.
Does Sleep Help Your Metabolism Improve?
Restricted Sleep and Metabolic Disorders
The link between restricted sleep and metabolic disorders is a focal point of research. As per recent research, continued sleep disruptions can cause lasting dysregulation in the neuro-endocrine system, impacting food intake and lipid metabolism, ultimately contributing to persistent metabolic disorders.
When individuals consistently experience insufficient sleep, their bodies undergo hormonal changes that can lead to increased hunger and disrupted appetite regulation. This imbalance is often characterized by increased levels of Ghrelin. This is the hormone that stimulates hunger. Further, sleep imbalances can reduce the body levels of Leptin, which is the hormone that provides a sense of satiety.
As a result, sleep-deprived individuals may find themselves more prone to overeating, especially high-calorie and carbohydrate-rich foods. The cumulative effect of these dietary choices can all lead to overall weight gain and you run the risk of developing metabolic disorders eventually.
How Is Physical Activity Interrelated To Sleep Hygiene?
It’s a Win-Win Equation!
Adequate sleep is integral to sustaining energy for physical activity and a good workout enhances your sleep quality. Sleep deprivation diminishes exercise readiness and safety, particularly for activities like weightlifting and those requiring balance. Though researchers continue to explore this connection, the well-established fact remains that exercise is crucial for weight management and overall health.
Research by National Institutes of Health (NIH) indicates that adults engaging in 30 minutes of daily exercise slept approximately 15 minutes more than non-exercisers. Additional studies highlight the positive impact of physical activity in alleviating sleep disorders like insomnia, daytime sleepiness, and sleep apnea
Regular exercise enhances sleep quality, especially when conducted in natural light. Even a brief daytime walk can positively impact sleep, but greater physical activity, such as at least 150 minutes of moderate-intensity or 75 minutes of high-intensity exercise per week, contributes to improved daytime concentration and reduced daytime sleepiness.
Obesity and Sleep Health: Bidirectional Relation
There is a bidirectional relation between obesity and disturbed sleep, meaning that not only does inadequate sleep contribute to weight gain, but excess weight can also disrupt sleep patterns. Conditions such as obesity and excess body fat often stem from causes like insomnia, sleep apnea and certain other sleep disorders. This creates a cyclical pattern where poor sleep and weight gain perpetuate each other.
Top 5 Tips to Improve Sleep & Promote Fast Weight Loss!
In this section I have reflected on my own individual experience on how I go to sleep faster. I have tried and tested several sleep hygiene practices and shared some tips for quality sleep to help in your weightloss plan.
- Tip 1: Follow a Sleep Schedule
Fluctuations in sleep patterns impact metabolism and insulin sensitivity, affecting blood sugar levels.
- Tip 2: Sleep in Darkness and Positions to Sleep
Exposure to artificial light, like from TVs or bedside lamps, is linked to an increased risk of weight gain and obesity. Try to identify a comfortable sleep position aligned with your body type and health conditions like body pain.
- Tip 3: Avoid Late-night Eating
Eating close to bedtime may hinder weight loss efforts.
- Tip 4: Manage Stress
Chronic stress disrupts sleep and can contribute to weight gain; finding healthy coping mechanisms is essential.
- Tip 5: Be an Early Riser
Late bedtimes are associated with higher calorie intake and increased risk of weight gain. Early risers are more likely to maintain weight loss compared to night owls.
Ongoing Debate & Future Research
While the existing research highlights the connection between sleep and weight, ongoing debates within the medical community revolve around the intricate details of this relationship. Researchers are exploring various avenues to better understand the complex interplay between sleep and weight regulation.
Some hypotheses suggest that circadian rhythm disruptions, which occur when the body’s internal clock is out of sync with external cues like daylight, may contribute to weight gain. Others propose that the impact of sleep on mood and energy levels influences food choices and physical activity, ultimately affecting weight.
Future research aims to uncover these nuances and explore potential interventions to improve both sleep quality and weight management. By gaining a deeper understanding of sleep deprived symptoms and the intricate mechanisms linking sleep and fast weightloss, researchers hope to develop more effective strategies for weight loss and obesity prevention.
Sleep Health & Wellness
Prioritizing sleep hygiene is integral to overall well-being and successful weight management. The evidence linking sleep and weight highlights the importance of adopting healthy sleep hygiene practices. Whether through establishing consistent sleep routines, creating a conducive sleep environment, or seeking professional help for sleep disorders, individuals can take proactive steps to ease falling to sleep and in turn, support their fast weightloss plans.
As our scientific communities unravel all complexities of this relationship, the integration of sleep health into weight management strategies holds promises for reducing obesity rates and improving overall public health.
Disclaimer
The information provided is general and not a substitute for professional advice. It does not intend to diagnose sleep or mental health issues. Prior to making any changes to your sleep routine, it is advisable to seek guidance from a healthcare professional.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3632337/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6196958/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10503965/#:~:text=Scientific%20literature%20shows%20that%20adults,15%2C19%2C20%5D.
- https://www.ncbi.nlm.nih.gov/books/NBK546705/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7914147/







