What Are The 5 Best Mattresses For Parasomnia? Find Out
Ever wondered why on some nights you act out your dreams?
At SmartMattressBuy.com, we’re diving into the intriguing world of parasomnia – those curious sleep behaviors that go beyond the ordinary.
Curious about the causes, types, symptoms, and how it affects both adults and children? Can the proper bedding help improve sleep?
Join us as we resolve the mysteries of parasomnia, one question at a time.
What Is Parasomnia?
Often parasomnia is defined as a sleep disorder where unusual physical events disrupt your sleep.
According to National Institute of Health (NIH), these events can happen before or during sleep, involving actions like sleepwalking, talking, or experiencing night-time terrors. Even though you’re genuinely asleep, you may talk or walk during sleep which may give an impression like you are awake to others.
Now what is parasomnia sleep disorder?
The term “parasomnia” covers a range of unusual sleep-related behaviors, such as sleepwalking and sleep paralysis, arising during the different sleep stages and transitions. Sleep disorder or Parasomnias, occurring during the transition between sleep stages, vary in characteristics and frequency. While more prevalent in children, these behaviors can affect individuals of any age.
But how is parasomnia caused? Let’s now learn more about the causes of parasomnia.
What Are The Potential Causes of Parasomnia?
The causes of parasomnias can be categorized into factors that disrupt sleep and other general health issues. Let’s discuss some common causes of parasomnia to help you with timely prevention of the disorder.
Health Factors
- Physical Conditions: Fever, head injury, pregnancy, menstruation
- Psychological Factors:Stress, alcohol or substance abuse, psychiatric illnesses like depression, anxiety, Post Traumatic Stress Disorder (PTSD).
- Genetic Predisposition:Family history of parasomnias increases the likelihood of getting affected.
- Inflammatory and Neurological Diseases:Conditions like Parkinson’s disease, Lewy body dementia, stroke, multiple system atrophy, multiple sclerosis, brain tumors, migraines, and spinocerebellar ataxia type three can eventually cause parasomnia, if left untreated.
Let’s now venture into the types of Parasomnia and learn whether children are more susceptible to the disorder than adults.
Issues Disrupting Sleep
- Incomplete Transition to Sleep:Difficulty moving from wakefulness to all the sleep stages.
- Sleep Disruption Factors:Lack of sleep, irregular schedules and sleep patterns (e.g., jet lag, shift work).
- Medications:Certain medications (e.g., benzodiazepines, antidepressants, antipsychotics, blood pressure drugs, anti-seizure medications) can lead to parasomnia.
- Medical Conditions:Restless leg syndrome, sleep apnea, pain, narcolepsy, sleep deprivation, circadian rhythm disorders, or periodic limb movement disorder can disrupt sleep cycle and cause parasomnia.
- Sleep-Wake Cycle: In children with parasomnias, an immature sleep-wake cycle may play a role in causing this sleep disorder.
Can a Bad Mattress Disrupt Sleep and Cause Parasomnia?
Poor mattress support can lead to spinal misalignment, increased discomfort, and inadequate support for preferred sleeping positions, all of which negatively impact sleep quality. A bad mattress can significantly disrupt sleep and contribute to parasomnias, which are abnormal behaviors during sleep such as sleepwalking, night terrors, and restless leg syndrome.
Certain mattresses can really help alleviate sleep disorders like parasomnia by providing proper spinal alignment, enhancing comfort, and supporting various sleeping positions. The best mattress for improving sleep varies for each individual, depending on factors like body type, sleeping position, and specific comfort needs.
Let me guide you on how to choose a supportive and comfortable mattress for yourself. You need proper sleep for maintaining healthy sleep patterns and preventing parasomnia.
Here’s my curated list.
5 Best Mattresses For Parasomnia – Quick Look
- Best Overall in Parasomnias: Stearns & Foster Estate
- Best Mattress For Back Pain: iSense Hybrid Premier
- Mattress For Stomach Sleepers With Parasomnias: Helix Dawn
- Best Mattress For Combination Sleepers: Purple Rejuvenate
- Best Mattress For Allergies in Parasomnia Patients: Avocado Green Mattress
Short Reviews – Top 5 Mattresses For Parasomnia
An uncomfortable mattress can lead to poor sleep quality.
Here are 5 mattresses that will help you sleep even with parasomnias and associated sleeping problems. I’ve listed features of all the models below.
1. Stearns & Foster Estate Mattress
Best in Overall Features to Combat Sleep Issues Related to Parasomnias
- Type:Hybrid
- Thickness:15 Inches
- Firmness:Soft, Medium, Firm, Pillow Top Feel
- Size of Mattress:King, California King, Queen, Twin XL, Full
Smart Mattress Buy’s Review
Stearns and Foster Estate Mattress stands out a decent luxury mattress in overall features for parasomnias. Its luxurious design and high-quality materials offer exceptional support and comfort, promoting better spinal alignment and reducing discomfort. This mattress is particularly effective for those suffering from sleep disorders, providing a stable and supportive sleep surface that can help minimize disturbances.
Feel
When lying on Stearns and Foster Estate Mattress, you’ll experience a plush, supportive feel that adapts to your body. The combination of gel-infused foam and innerspring coils ensures a balance of comfort and support, providing a soothing sleeping surface that enhances relaxation and reduces pressure points.
Pros
- Good Core Support: The hybrid design with innerspring coils and gel-infused foam offers excellent support and spinal alignment.
- Luxurious Comfort: Plush pillow top and high-quality materials provide a luxurious feel.
- Durability: High-density foams and reinforced edges enhance durability and longevity.
- Cooling Technology: Gel-infused memory foam helps regulate temperature and keep you cool throughout the night.
- Motion Isolation: Reduces motion transfer, making it ideal for couples.
Cons
- Price: Higher price point compared to other mattresses.
- Weight: Heavier than many mattresses, which can make moving and setup more challenging.
- Firmness: May be too firm for those who prefer a softer sleeping surface.
Now, if you have the curiosity to know more about this mattress – Read Stearns & Foster Estate Mattress Review
2. iSense Hybrid Premier Mattress
Best Mattress For Back Pain in Parasomnia Patients
- Type:Hybrid
- Thickness:5 Inches
- Firmness:Adjustable (Customizable)
- Size of Mattress:King, California King, Queen, Twin XL
Smart Mattress Buy’s Review
iSense Hybrid Premier Mattress stands out as a versatile choice for customizable comfort. Combining pocket coils with iSense® open-cell foam, it offers exceptional pressure relief and support. Available in Standard, Flexhead, and Split variants, it caters to diverse sleep preferences and needs.
Feel
iSense Hybrid Premier Mattress provides a balanced feel with responsive coils and plush foam layers. It ensures comfort without excessive sinkage.
Pros
- Customizable firmness settings (20 options)
- Good pressure relief and support
- Cooling properties with gel-infused foam
- Responsive coil system for motion isolation
- CertiPUR-US® certified materials
Cons:
- Higher price point
- Heavier weight may make moving or adjusting difficult
If you’re eager to learn more about this mattress, delve into iSense Hybrid Premier Mattress Review.
3. Helix Dawn
Mattress For Stomach Sleepers With Parasomnias
- Type:Hybrid
- Thickness:5 inches
- Firmness:Firm
- Size of Mattress:Twin, Twin XL, Full, Queen, King, CA King
Smart Mattress Buy’s Review:
Helix Dawn Mattress is tailored for stomach sleepers and those experiencing parasomnias, combining targeted support and comfort. Engineered with premium materials, it aims to enhance sleep quality through personalized design and firmness options.
Feel:
Helix Dawn Mattress offers a firm feel, providing robust support to maintain spinal alignment for stomach sleepers. It contours enough to relieve pressure points without excessive sinkage, ensuring a balanced and comfortable sleep surface.
Pros:
- Tailored for stomach sleepers with a firm feel that supports spinal alignment.
- Customizable options to match individual preferences and sleep styles.
- Enhanced pressure relief and motion isolation for undisturbed sleep.
Cons:
- May feel too firm for those who prefer softer mattresses.
- Initial off-gassing odor reported by some users.
- Limited availability in physical stores, primarily sold online
For more information, head on to our Helix Dawn mattress review page.
4. Purple Rejuvenate
Best Mattress For Combination Sleepers
- Type:Hybrid
- Thickness:5 inches
- Firmness:Firm
- Size of Mattress:Twin XL, Queen, King, Cal King, Split King
Smart Mattress Buy’s Review
The Purple Rejuvenate Mattress is hailed as the ideal choice for combination sleepers, offering a unique blend of support and comfort. Its innovative Purple Grid™ technology adapts dynamically to various sleeping positions, ensuring a restful night’s sleep.
Feel
When lying on the Purple Rejuvenate Mattress, sleepers experience a balanced feel of responsiveness and support. The Purple Grid™ contours gently to the body, providing pressure relief where needed while maintaining a buoyant and comfortable surface.
Pros
- Versatile Support: Adapts well to different sleeping positions.
- Pressure Relief: Effectively relieves pressure points.
- Cooling Technology: Promotes airflow and temperature regulation.
Cons
- Firmness: Might feel too firm for those preferring a plush feel.
- Edge Support: May lack robust support around the edges compared to traditional mattresses.
Check out our detailed Purple Rejuvenate mattress review page for additional information.
5. Avocado Green Mattress
Best Mattress For Allergies in Parasomnia Patients
- Type:Hybrid
- Thickness:11 inches
- Firmness:Firm
- Size of Mattress:Twin, Twin XL, Full, Queen, King, California King
Smart Mattress Buy’s Review
Avocado Green Mattress is highly recommended by Smart Mattress Buy for allergy sufferers and parasomnia patients. It combines organic materials with a natural latex comfort layer, providing excellent support and comfort while minimizing allergens and disturbances that can affect sleep quality.
Feel
Avocado Green Mattress offers a firm feel with a gentle bounce, thanks to its latex and coil hybrid design. When lying on it, you’ll experience a supportive yet responsive sensation that conforms to your body’s contours, offering pressure relief and a balanced sleep surface.
Pros
- Made with organic materials, including GOTS-certified organic cotton and natural latex.
- Provides excellent support and comfort for all sleep positions.
- Minimizes allergens with its natural materials and non-toxic certification.
- Features a durable construction with reinforced edge support.
- Offers optional pillow-top for added comfort.
Cons
- May feel too firm for some sleepers who prefer a softer mattress.
- Higher price point compared to some conventional mattresses.
- The natural latex may have a slight odor initially.
- Heavyweight due to its organic and durable materials.
Visit our comprehensive Avocado Green mattress review page for more details.
Mattress prices fluctuate based on demand, supply, and seasonal promotions, For the latest offers and discounts, visit our “Best Time to Buy a Mattress” page. Don’t miss out—grab the suitable mattress at the best price now!
Now that we’ve covered everything about sleep and mattresses, let’s delve into this sleep disorder and learn about its types.
Are There Several Types of Parasomnia?
1. REM-Related Parasomnia
REM sleep, or Rapid Eye Movement sleep, is a phase where the brain is highly active, eyes move rapidly, and muscles are briefly paralyzed. We dream mostly during REM sleep. REM-related parasomnias involve sleep disruptions like muscle paralysis irregularities.
- REM Sleep Behavior Disorder (RSBD)
In RSBD, people act out their dreams with unusual movements or vocalizations during REM sleep. It’s often linked to actions like kicking or yelling, commonly observed in individuals with Parkinson’s disease.
- Sleep Paralysis
During sleep paralysis, individuals briefly lose the ability to move while falling asleep or waking up. This may be accompanied by hallucinations or a feeling of suffocation. While not harmful, it can cause anxiety in the later stages.
- Nightmare Disorder
Nightmare disorder involves recurrent, vivid nightmares leading to fatigue and distress. Those with PTSD often experience this condition. While occasional bad dreams are normal, persistent and distressing nightmares may indicate nightmare disorder. Even this can lead to parasomnia and lack of revitalizing sleep.
2. NREM-Related Parasomnia
Non Rapid Eye Movement (NREM) sleep encompasses the initial 3 stages of sleep, occurring during the first half of the night. NREM sleep disorders, often termed as arousal disorders, involve physical and verbal activities without complete awareness. These typically affect individuals aged 5 years to 25 years, and manifest in those with a family history of similar issues.
Parasomnias during NREM sleep include,
Sleepwalkers, though seemingly awake with open eyes, engage in activities while asleep. This may include complex tasks or unusual actions, posing risks such as injury due to lack of wakefulness or awareness of surroundings.
- Nighttime Terrors
These terrors are characterized by sudden awakening in a terrified state, accompanied by screaming or crying. Brief but intense, they last up to a few minutes and involve features like racing heart, dilated pupils, breathlessness, and sweating.
- Confusion-related Arousals
Individuals with this disorder appear partially awake but may experience confusion and disorientation regarding time and space. Episodes may involve sitting up, open eyes, slurry speech, and difficulty understanding or responding coherently. Common in childhood, these tend to decrease with age.
- Sleep-related Eating Disorder
It involves eating and drinking while partially awake during sleep. Individuals may consume unusual or inappropriate foods, posing risks such as ingesting toxic substances, overeating, or sustaining injuries during food preparation.
Non-REM parasomnias reflect a complex interplay of genetic and environmental factors, with potential dangers arising from unaware and partially awake behaviors during sleep.
3. Other Types of Parasomnia
Apart from the aforementioned types of parasomnias, we have discussed a few more types below.
- Hallucinations
This disorder involves experiencing hallucinations while falling asleep or waking up. Individuals may see, hear, feel, or sense movement that isn’t real, and in some cases, they may even leave their bed to escape the perceived experiences.
- Sleep-Related Groaning
This is also referred as Catathrenia and people produce repetitive episodes of groaning noises during sleep. These may consist of long groans followed by sighs or grunts.
- Sexsomnia
This sleep disorder involves engaging in sexual behaviors during sleep. These behaviors can include intercourse, masturbation, sexual assault, fondling of a bed partner, or sexual vocalizations. Sexsomnia poses challenges not only to the individual experiencing it but also to those sharing a sleep environment.
- Exploding-Head-Syndrome
Individuals with this sleep disorder perceive a loud noise or explosive crashing sound in their head as they fall asleep or wake up. This may be accompanied by an imaginary flash of light or a sudden muscle jerk.
- Sleep Enuresis
Unlike common bedwetting in young children, parasomnia-related bedwetting occurs in children aged 5 and older, happening at least two times a week for a stretch of 3 months.
Each of these parasomnias reflects distinct disturbances in sleep patterns and can impact the overall quality of sleep, as well as the well-being of those affected and those around them.
Is There An Interrelation B/w Parasomnia and Children?
You may wonder if parasomnias affect children and even if it is so, how prevalent is the occurrence in children.
Well, parasomnias have a higher prevalence in children compared to adults.
- Among children under the age of 15 years, non-REM sleep disorders are more prevalent than REM disorders.
- The most frequently observed parasomnias in this age group include confusion-based arousal, sleepwalking, sleep terror, and nightmares.
- Notably, children with neurological or psychiatric health conditions, such as epilepsy, Attention-Deficit Hyperactivity Disorder (ADHD), or developmental issues, are more prone to experiencing parasomnias.
Thus we can clearly see a connection between certain health challenges and the occurrence of parasomnias in children.
Are Parasomnias Related to Gender Too?
The prevalence of parasomnias exhibits gender-specific patterns.
- Nightmares tend to occur more frequently in females, while sexsomnia is observed more commonly in males.
- REM sleep behavior disorder is predominantly reported in males aged 50 years and above.
- On the other hand, sleep terrors, confusion-based arousals, and sleepwalking exhibit similar occurrences in both males and females.
These variations underline the distinct ways in which parasomnias may manifest across genders.
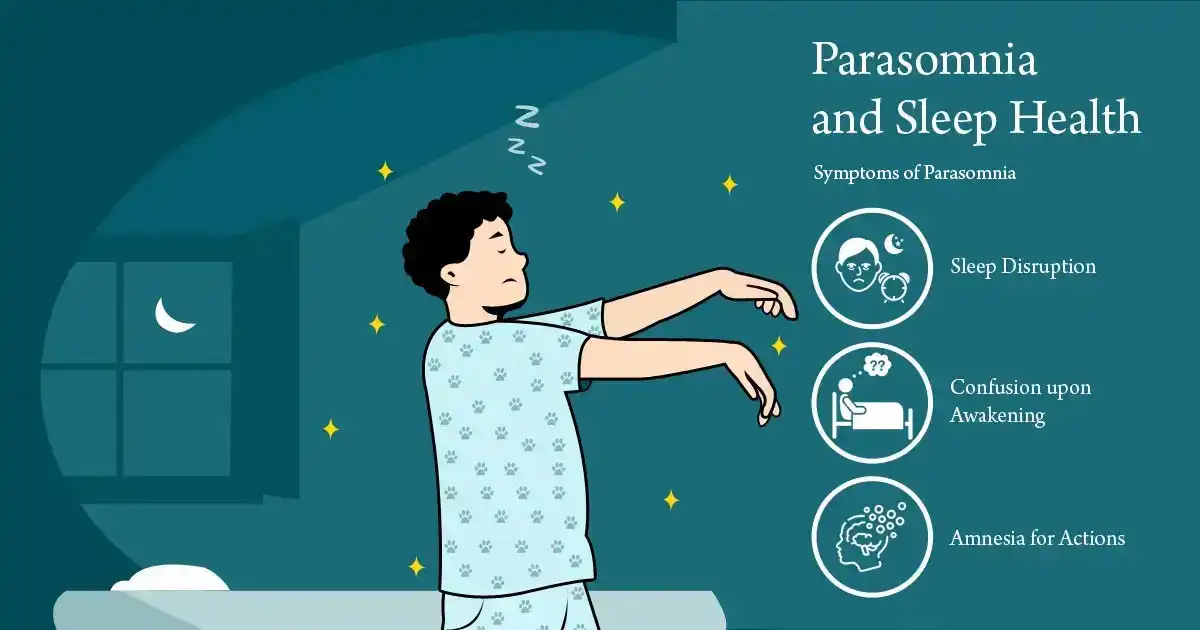
Symptoms of Parasomnia
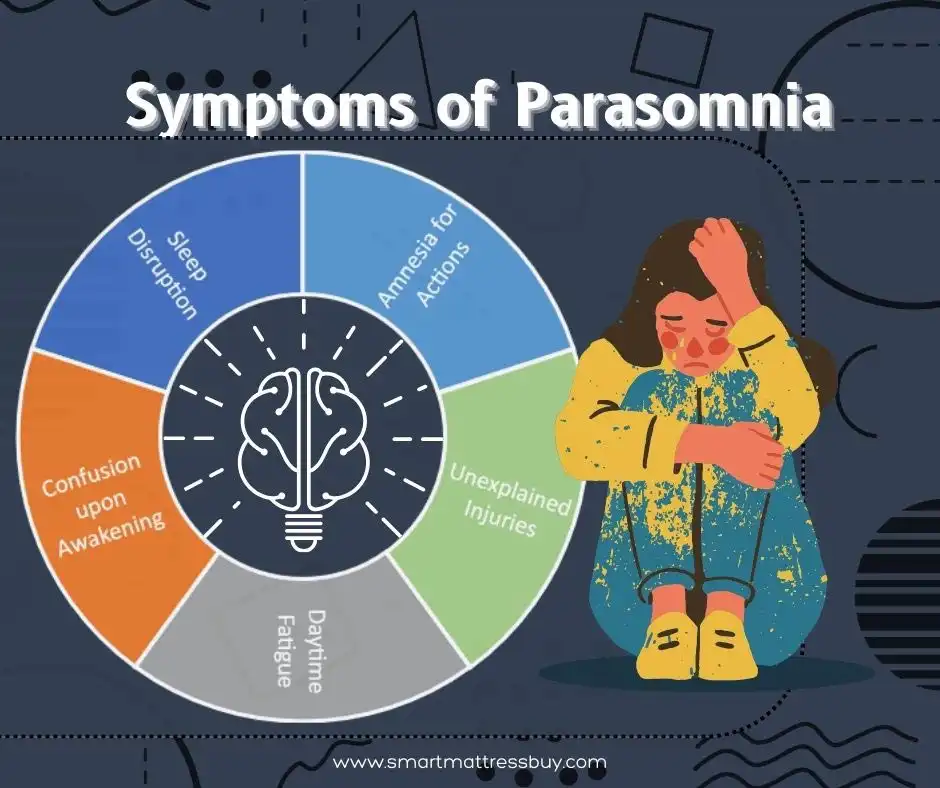
In the above sections we discussed about several types of parasomnia and the causes behind it. Do these types have some symptoms in common?
Yes, there are some symptoms common to all these types of sleep disorder & parasomnia. Timely identification of these parasomnia symptoms can help you identify the person at risk and take the necessary treatment measures.
These are some common symptoms that individuals with parasomnia may experience:
- Difficulty in Sleeping Through the Night: Persistent challenges in maintaining uninterrupted sleep.
- Wake up Disoriented: Another frequent symptom involves waking up with a sense of confusion or disorientation.
- Daytime Fatigue: Experiencing tiredness and fatigue during the day, often due to disrupted sleep patterns.
- Unexplained Cuts and Bruises: Discovering injuries on the body for which there is no recollection of the cause, indicating certain physical activity during sleep.
- Unaware Movements, Expressions, Vocalizations, or Activities:Engaging in movements, facial expressions, vocalizations, or activities during sleep, as reported by a sleep partner, without personal recollection of these actions.
These parasomnia symptoms collectively reflect the diverse and often puzzling nature of parasomnias. This type of sleeping disorder can impact both your quality of sleep and daily life functioning.
Now, that we have learnt about the parasomnia symptoms lets guide you through the diagnostic procedures and treatment involved.
How Can We Diagnose Parasomnia?
The diagnosis involves a comprehensive assessment by a sleep medicine specialist. The procedure involves several elements to gain a thorough understanding of an individual’s sleep symptoms.
We have detailed the diagnosis process for your help and understanding.
- Clinical Evaluation
A medical practitioner interviews the concerned individual and their sleep partner in order to gather information about sleep symptoms. Details about medical history, family history, alcohol use, substance abuse, and current medications are further explored.
- Sleep Diary
Individuals are asked to maintain a sleep diary of their own to document their sleep patterns and any parasomnia related events. Additionally, the sleep partner may be requested to keep track of observed sleep events.
- Sleep Study (Polysomnogram)
Conducted in a sleep laboratory, this study monitors an individual during sleep. Parameters such as brain waves, heart rate, eye movements, and breathing are recorded, while video captures movements and behaviors. Although some sleep studies can be conducted at home, a medical practitioner can recommend in-lab study if there is concern for parasomnia.
- Video Electro-Encephalo-Gram (EEG)
Healthcare providers can now visualize and record brain activity during specific events. This aids in the diagnosis of parasomnias.
- Neurologic Tests and Imaging
Additional tests, such as a neurologic exam or imaging scans (CT scan or MRI), are also often employed to detect any degeneration of the brain. Medical practitioners can thus detect any underlying neurologic cause contributing to symptoms of parasomnia.
A combination of these diagnostic tools enables sleep specialists to draw a comprehensive understanding of parasomnia. By identifying potential causes of this sleep disorder, a practitioner can finally formulate an appropriate treatment plan.
Parasomnia & Its Treatment
How is Parasomnia treated? Can parasomnia be cured?
Well, the treatment of parasomnia involves a comprehensive approach. It starts with identification and management of underlying sleep problems, addressing associated health issues, and reviewing medications that may trigger parasomnia.
Non-REM and REM Related Treatment
- Good Sleep Hygiene Habits
- Aim for 7-9 hours of sleep per night.
- Turn off lights, TV, and electronic devices before bedtime.
- Maintain a cool room temperature conducive to sleep.
- Avoid caffeine and strenuous exercise close to bedtime.
- Consistent Sleep-Wake Schedule
- Establish and adhere to a regular bedtime and wake-up time.
- Limit Alcohol and Recreational Drugs
- Restrict or avoid the use of alcohol and recreational drugs.
- Take Prescribed Medications
- Adhere to the prescribed medication regimen under the guidance of a healthcare provider.
Additional Parasomnia Treatments & Management Strategies
- Non-REM Parasomnia
- Medication-based Treatment:Benzodiazepines, particularly for long-lasting or potentially harmful parasomnias. Tricyclic antidepressants may also be considered.
- Psychological Treatment: Hypnosis, relaxation therapy, cognitive-behavioral therapy, or psychotherapy may be employed.
- REM Parasomnia
- Medication-based Treatment: Clonazepam and melatonin are commonly used to manage REM sleep disorders.
Safety Measures & Helpful Tips
- Environment Modification
- Remove dangerous or sharp items from the bedroom.
- Secure tableside lights and pad the edges of bedside furniture.
- Use plastic bottles and cups if water is needed at the bedside.
- Install alarms on windows and doors for sleepwalkers.
- Sleeping Arrangements
- If aggressive behaviors are displayed, such as punching or kicking, consider sleeping in separate beds for safety.
It is up to a medical practitioner to select an appropriate treatment strategy – be it medications or psychological approaches, and tailor it depending on the specific type of parasomnia.
Additionally, a practitioner takes into account an individual’s unique health history and medical conditions. However, you need to remember that regular communication with a healthcare provider is crucial for ongoing evaluation and adjustment of the prescribed treatment plan.
What Are The Treatment Procedures of Parasomnia in Children?
In children, occurrences of parasomnia, especially Non-REM parasomnias are most prevalent during childhood and often naturally resolve during adolescence.
In many cases, the primary intervention process involves providing calming reassurance to the child from their parents, assuring them that everything is okay. Medications are rarely deemed necessary in parasomnia treatments or in the management of childhood parasomnias.
However, if medication is considered, it is typically prescribed for a limited duration, ranging from 3 to 6 weeks. Benzodiazepines or anti-anxiety drugs are common medications that are tried to mitigate the symptoms and better sleep quality.
Medications should be used cautiously understanding that childhood parasomnias often have a transient nature and may resolve with time and family reassurance.
Overall, the treatment of parasomnia in children emphasizes on conservative and supportive measures. Medication is recommended only in specific cases and for a limited duration under the supervision of healthcare professionals.
Further, regular communication with healthcare providers is essential to monitor a child’s progress and make any necessary adjustments to the treatment plan.
Prevention of Parasomnia
While some causes of parasomnias, such as those stemming from neurological diseases, mental health issues, or heredity, may be challenging to prevent, there are proactive measures that you can adopt to mitigate the risk of developing or exacerbating parasomnias.
Preventive Strategies
These preventive measures align with the treatment approaches that we discussed earlier. Let’s discuss.
- Adequate Sleep Duration
Aim for seven to nine hours of sleep per night to support overall sleep health.
- Consistent Sleep Schedule
Maintain a regular sleep-wake schedule with consistent bedtime and wakeup times, promoting a stable sleep routine.
- Limiting Substance Use
Restrict or avoid the use of alcohol and drugs, as these substances can interfere with sleep patterns.
- Medication & Assessment
Consult with a healthcare provider to review and assess the impact of current medications on sleep. Certain medications may disrupt sleep, and if identified, alternative drugs or adjustments to the prescription may be considered.
By incorporating these preventive measures into one’s lifestyle, individuals can create a sleep-friendly environment and potentially reduce the likelihood of experiencing parasomnias.
Proactive management, along with regular communication with healthcare providers, can play a crucial role in minimizing the impact of parasomnias and promoting overall sleep quality.
When to Consult Medical Practitioner?
It is advisable to consult a medical practitioner if you or a family member experiences any abnormal sleep-related behaviors, particularly those associated with injuries or disruptions in sleep.
Some key signs that warrant a discussion with a doctor include:
- Injuries During Sleep
If there are unexplained injuries, cuts, or bruises on yourself or a family member, especially those that occur during sleep.
- Disruption of Sleep Patterns
Are you suffering from persistent disruptions in sleep? Sleep disruptions like frequent awakenings, nightmares, or unusual movements during the night must be given importance to.
- Changes in Behavior
Observable changes in behavior during sleep, as reported by a bed partner, including movements, vocalizations, or activities that are not remembered upon waking.
- Sleep-Related Distress
If abnormal sleep-related behaviors are causing distress, impairment in daily functioning, or negatively impacting your overall quality of life.
- Family History
A family history of sleep disorders or parasomnias may also trigger parasomnia. Ensure to have a discussion with a medical practitioner. Timely consultation with a healthcare professional is essential to assess the nature of the sleep-related behaviors.
Acting on time can help you to identify potential underlying causes, and determine an appropriate course of action.
Addressing these concerns promptly can lead to effective diagnosis and management of parasomnia or any other sleep disorders.
Disclaimer:
The information provided is for general informational purposes and should not be considered a substitute for professional advice. It does not aim to treat, diagnose, or cure any sleep or mental health conditions. Before making any changes to your sleep or mental health regimen, it is recommended to consult with a qualified healthcare professional.
References
- Acharya, J.N. and Acharya, V.J., 2024. REM parasomnias: Straddling the sleep-wake line. Clinical Neurophysiology Practice, 9, p.51.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10847008/
- Gavidia, R., Whitney, D.G., Hershner, S., Selkie, E.M., Tauman, R. and Dunietz, G.L., 2022. Gender identity and transition: relationships with sleep disorders in US youth. Journal of Clinical Sleep Medicine, 18(11), pp.2553-2559.
https://jcsm.aasm.org/doi/full/10.5664/jcsm.10158
- Senel, G.B., Kochan Kizilkilic, E. and Karadeniz, D., 2021. Restless sleep disorder in children with NREM parasomnias. Sleep, 44(7), p.zsab049.
https://academic.oup.com/sleep/article-abstract/44/7/zsab049/6149528
- Bollu, P.C., Goyal, M.K., Thakkar, M.M. and Sahota, P., 2018. Sleep medicine: parasomnias. Missouri medicine, 115(2), p.169.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6139852/
- Sabater, L., Gaig, C., Gelpi, E., Bataller, L., Lewerenz, J., Torres-Vega, E., Contreras, A., Giometto, B., Compta, Y., Embid, C. and Vilaseca, I., 2014. A novel NREM and REM parasomnia with sleep breathing disorder associated with antibodies against IgLON5: a case series, pathological features, and characterization of the antigen. Lancet neurology, 13(6), p.575.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4104022/
- Howell, M.J., 2012. Parasomnias: an updated review. Neurotherapeutics, 9(4), pp.753-775.
https://www.sciencedirect.com/science/article/pii/S1878747923017178








